Estimated reading time: 13 minutes
Does critical limb ischemia (CLI) trap you?
Imagine walking again, pain-free, with renewed energy.
Mesenchymal stem cell (MSC) therapy tackles the root of CLI, promoting blood flow, healing wounds, and alleviating pain.
MSC therapy boosts ankle pressure by 40%, suggesting improved blood flow, an 800% increase in walking distance, and an 80% reduction in agonizing rest pain.
Table of contents
- Critical Limb Ischemia: A Ticking Clock on Your Legs
- Improving Blood Flow in CLI: The Role of MSC Therapy
- How MSCs Build New Blood Vessels in CLI?
- MSC therapy reduces CLI Leg Pain
- The Relationship Between Leg Edema and MSCs in Chronic Limb Ischemia
- The potential link between MSC therapy and skin discoloration in CLI
- MSC therapy can help reduce nerve pain in people with Critical Limb Ischemia
- The amputation risk in CLI
- Critical limb ischemia and death
- Critical Limb Ischemia, MSC therapy, and mindful living
- FAQ
Critical Limb Ischemia: A Ticking Clock on Your Legs
Your legs may be in danger due to Critical Limb Ischemia (CLI). It occurs when your limbs don’t get enough oxygen and nutrition, leading to severe pain, swelling, wounds, and even amputation. However, recognizing the warning signs can help save your legs.
Here are some signs to look out for
Blood Supply
- Cold and clammy feet: CLI can make your feet feel like icy daggers.
- Paleness or discoloration: If your skin looks pale, bluish, or mottled, it could be a red flag.
- Weak or absent pulses: Check your pulse at the ankle or foot. If it’s faint or missing, it could spell trouble.
Pain
- Rest pain: CLI causes constant burning, aching, or throbbing pain.
- Night pain: The pain intensifies in the darkness, making sleeping difficult.
- Burning sensation: If your leg feels on fire, it could signify danger.
Edema
- Swollen legs and ankles: Fluid build-up due to poor circulation creates discomfort and puffiness.
Skin changes
- Shiny, taut skin, hair loss, and blisters can signal tissue damage from swelling.
Ulcers that won’t heal
- Open wounds that refuse to close are a dire warning of tissue death.
Amputation Threat
- Gangrene: Dead tissue turns black and can spread quickly.
- Infection: Open wounds invite infections, further jeopardizing limbs and life.
Loss of mobility
- As CLI progresses, you may lose mobility and become unable to walk.
If you notice any of these symptoms, don’t wait – seek medical help immediately. Remember, early detection and prompt treatment can prevent the worst outcomes of CLI.
Improving Blood Flow in CLI: The Role of MSC Therapy
MSCs weave new blood vessels, bringing oxygen and life back to starved tissues and easing pain and swelling.
It is done by immunomodulation and angiogenesis.
Reducing Inflammation with MSCs
MSC therapy targets key players in the inflammatory response, reducing inflammation and promoting healing in patients with Critical Limb Ischemia.
Effectively controlling an overactive immune system
MSCs specifically target and neutralize key players in the inflammatory response, such as dendritic cells, T cells, and macrophages.
By effectively putting the brakes on dendritic cell activity, MSCs prevent them from activating other immune cells, such as T and NK cells.
Furthermore, MSCs have the ability to directly interact with T cells, efficiently halting the production of inflammatory molecules like TNF-α and IFN-γ.
In fact, they even promote the development of regulatory T cells, which have a critical role in maintaining a healthy immune system.
MSCs also effectively reduce macrophage aggression by inhibiting the release of pro-inflammatory factors and enhancing their cleanup abilities.
Moreover, they steer macrophages towards an anti-inflammatory M2 phenotype, which promotes healing and tissue repair.
Multi-Stage Action
Did you know that Multi-Stage Action is crucial for a complete healing process?
MSCs are known for their ability to not only stop inflammation but also to promote healing. How do they do it, you ask?
Well, it’s simple. First, MSCs work hand in hand with macrophages to remove any cellular debris left behind. This is done by promoting phagocytosis, a natural process that helps eliminate unwanted waste.
Second, MSCs secrete growth factors that are essential for tissue regeneration. These growth factors help pave the way for recovery, making it possible for the leg to heal and function again.
Beyond inflammation
MSCs also directly interact with smooth muscle cells to promote anti-inflammatory processes and accelerate healing.
This is particularly important in the context of CLI treatment.
How MSCs Build New Blood Vessels in CLI?
MSCs restore blood flow in CLI by crafting new blood vessels through growth factors, reducing inflammation and cell recruitment.
They do this through several remarkable feats
Growth Factor secretion
MSCs pump out growth factors like VEGF, bFGF, and HGF. These “magic potions” wake up dormant endothelial cells, the building blocks of blood vessels.
Endothelial cells multiply, migrate, and form tubes, eventually becoming new blood vessels that bring life back to your leg.
Calming the Inflammation
MSCs release IL-10 and PD-L1, which calm down immune cells called dendritic cells. It creates a friendly environment for new vessels to grow without being attacked.
Influence on T cells
MSCs also influence T cells and convince them to produce IL-10.
The IL-10 is another peacekeeper, calming down inflammation and making it easier for new vessels to sprout.
Macrophage Makeover
MSC rereleases IL-10, a substance that changes the behavior of macrophages. As a result, macrophages release growth factors to help grow new blood vessels.
Activating Progenitors
Endothelial progenitor cells (EPCs) act as blood vessel builders.
MSCs release VEGF and SDF-1 signals. These signals activate endothelial progenitor cells (EPCs) and recruit them to help build blood vessels.
Nourishing Progenitors
MSCs don’t just recruit EPCs; they nurture them too. They release growth factors like IGF-1 and HGF, providing nutrients for the young vessels to grow strong.
Guiding Progenitors
MSCs act like mentors, guiding EPCs to mature into fully functional blood vessels. IL-10 plays a crucial role here, helping EPCs reach their full potential as builders of a healthy, revitalized blood network.
MSCs become the architects of a new blood supply in your leg, bringing back oxygen, nutrients, and hope.
By all means,
MSC therapy effectively restores blood flow in the lower extremities of patients with Critical Ischemia.
How is blood flow measured in the limb?
Ankle systolic pressure in CLI
The systolic pressure in the ankle region measures the severity of CLI.
In patients with CLI or PAD, the ankle systolic pressure is often reduced due to arterial blockage and decreased blood flow in the lower extremities.
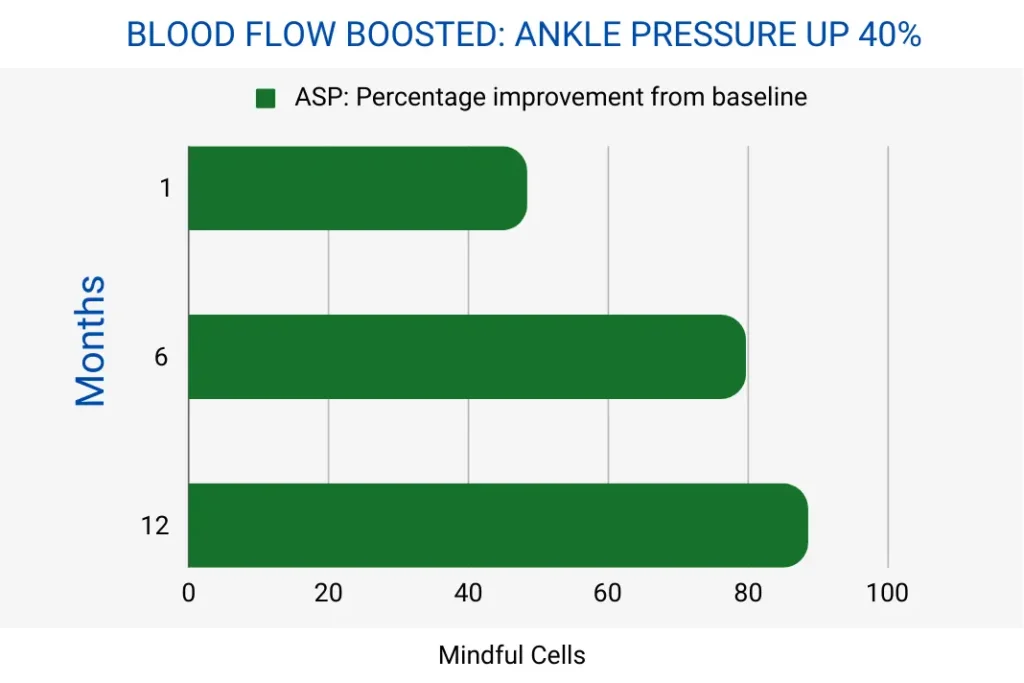
MSC Therapy Push Ankle Pressure 40% higher in 12 months, suggesting improved blood flow.
Results demonstrated in a clinical study with ‘No Option’ for treating critical limb ischemia patients.
Ankle-brachial pressure index in CLI
In CLI patients, the Ankle-brachial pressure index (ABPI) is an essential diagnostic tool to evaluate the blood flow and arterial blockage in the lower limbs.
A lower ABPI value indicates a higher degree of arterial blockage and reduced blood flow in the lower extremities, characteristic of CLI.

MSC therapy increases ankle-brachial pressure index by over 40% in 12 months, suggesting improved blood flow
Results demonstrated in a Phase III clinical trial with ‘No Option’ for treating critical limb ischemia patients.
MSC therapy reduces CLI Leg Pain
Improved blood flow and reduced inflammation significantly reduce CLI leg pain.
Improving blood flow can help reduce pain
The primary cause of pain in CLI is the lack of oxygen and nutrients reaching leg tissues due to clogged or insufficient blood vessels.
- MSC therapy mediated new blood vessel growth improves blood flow, delivering essential oxygen and nutrients, directly addressing the source of pain and leading to significant pain reduction.
Improved blood flow from new vessels promotes tissue repair and regeneration, preventing further damage and potentially healing existing wounds.
- Wound healing ultimately reduces pain associated with tissue injury and inflammation.
Muscles need adequate oxygen and nutrients to function correctly. When deprived, they become weak and can quickly fatigue, causing pain.
- New blood vessels increase oxygen and nutrient supply to the leg muscles, improving their function and reducing pain from fatigue or overuse.
Immunomodulation helps to reduce pain in CLI
Chronic inflammation in CLI contributes to pain and tissue damage.
Overactive immune responses can hinder blood vessel formation and worsen pain.
- MSCs calm the T-cell immune system, promote better vessel growth, and reduce inflammation-related pain.
- MSCs turning macrophages into M2 phenotype promote healing and tissue repair, reducing inflammation and tissue damage pain.
By all means, MSCs reduce inflammation, create a more favorable environment for new blood vessel growth, and prevent further tissue damage, reducing pain.

MSC therapy can reduce pain by 80% in 12 months by improving blood flow and reducing inflammation in Chronic Limb Ischemia.
Results demonstrated in a Phase III clinical trial with ‘No Option’ for treating critical limb ischemia patients.
The Relationship Between Leg Edema and MSCs in Chronic Limb Ischemia
There is a solution to the leg edema.
The combined effects of reduced inflammation, improved blood flow, lymphatic drainage, and tissue repair work together to minimize leg edema effectively.
Reduced Inflammation and leg edema
Inflammation significantly contributes to fluid leakage from blood vessels and edema formation.
- However, MSCs target key players like dendritic cells, T cells, and macrophages, reducing their production of pro-inflammatory molecules like TNF-α and IFN-γ. Consequently, inflammatory response dampens and reduces the associated edema.
- MSCs release IL-10 and PD-L1, which promote regulatory T cells and M2 macrophages, actively suppressing inflammation and enhancing lymphatic drainage. As a result, it reduces tissue build-up.
Improved Blood Flow and Lymphatic Drainage
- New blood vessels created by MSC therapy improve blood circulation. Hence, venous system pressure reduces and minimizes fluid leakage into tissues.
- MSCs also stimulate the formation of new lymphatic vessels, promoting improved lymphatic drainage and reducing edema.
Tissue Repair and Edema
- MSCs secrete growth factors that reduce excessive scarring and promote tissue repair.
- Consequently, improved tissue structure enhances lymphatic drainage and reduces fluid accumulated in the damaged areas.
- Ultimately, it leads to a significant decrease in leg edema.
The potential link between MSC therapy and skin discoloration in CLI
MSC therapy can improve blood flow and reduce inflammation in CLI, leading to better skin health.
- It can help balance the production of melanin by skin cells.
- Prevent scarring and thickening of the skin, and make the skin smoother.
- MSC therapy can also reduce the skin thickening caused by fibrosis.
- MSC therapy improves the skin tone and texture by reducing edema or fluid accumulation.
MSC therapy can help reduce nerve pain in people with Critical Limb Ischemia
Neuropathy is a condition where there is damage to the nerves in the legs. Neuropathy causes pain, numbness, and tingling.
The nerve damage in legs is often caused by poor blood flow and chronic inflammation.
Addressing the Underlying Cause of Neuropathy
MSCs control the overactive immune system, which is responsible for the inflammation that damages the nerves.
Protecting Nerves from Further Damage
MSCs also protect nerves from further damage by releasing anti-inflammatory substances IL-10 and PD-L1 that reduce inflammation.
These anti-inflammatory factors also promote the growth of new blood vessels, which help provide essential nutrients and oxygen to the nerves.
Supporting Nerve Repair
Lastly, MSCs can help with nerve repair. MSCs release IGF-1 and HGF growth factors that stimulate nerve growth and repair.
The amputation risk in CLI
CLI causes wounds and sores that don’t heal and might lead to amputation of the affected limb. However, there are ways to prevent the risk of amputation.
Firstly, let’s address the underlying cause of CLI.
- Promoting new blood vessel formation and suppressing inflammatory pathways protect tissues from further damage and reduce the need for amputation.
Secondly, MSC therapy enhances wound healing capacity, preventing further tissue loss and making limb salvage possible.
- Yes, MSC therapy helps heal wounds significantly in CLI patients.
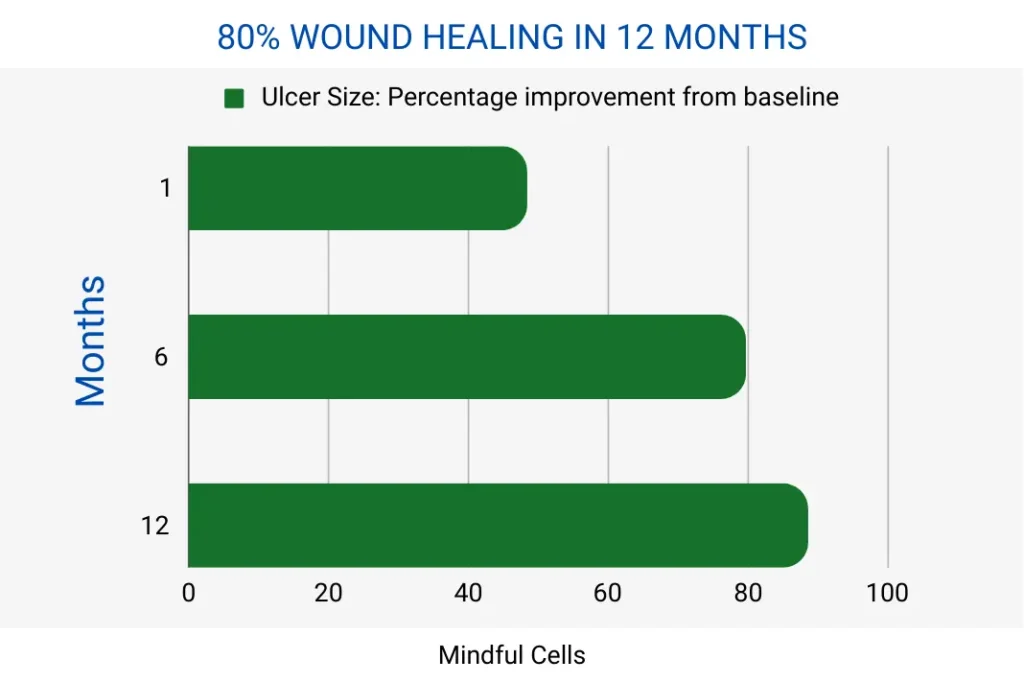
MSC therapy heals wounds by 80% in 12 months in CLI patients
Results demonstrated in a Phase III clinical trial with ‘No Option’ for treating critical limb ischemia patients.
Moreover, MSC therapy reduces pain and fatigue and improves walking ability. This can significantly improve the quality of life for those with CLI and help prevent the need for amputation.
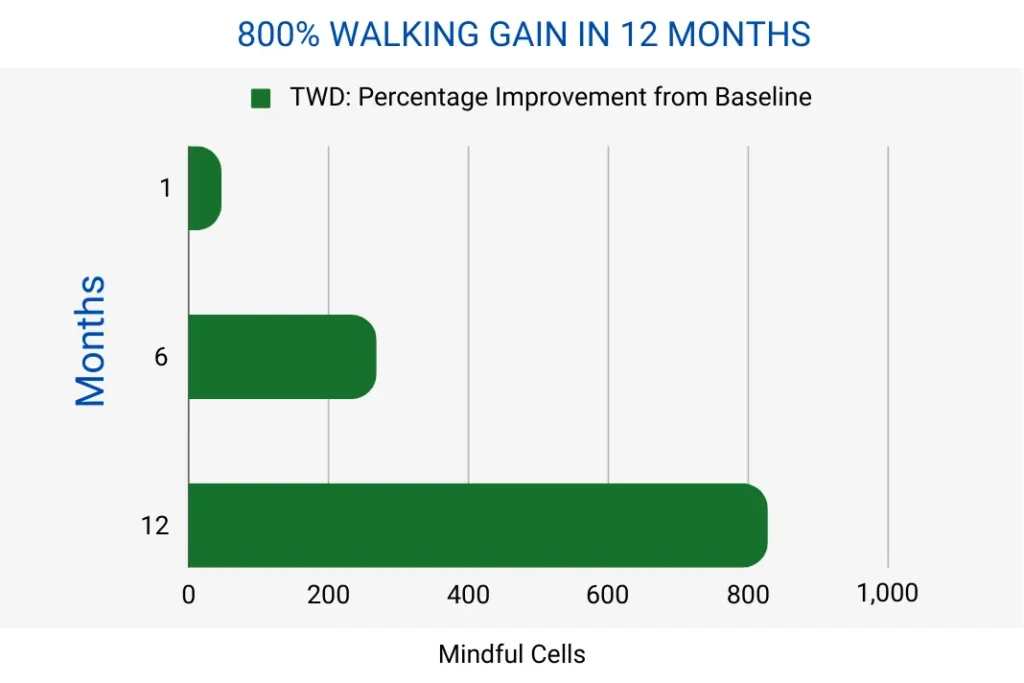
MSC therapy boosts walking by 800% in CLI patients in 12 months
Results demonstrated in a Phase III clinical trial with ‘No Option’ for treating critical limb ischemia patients.
Critical limb ischemia and death
MSC therapy works by treating the underlying problem causing CLI, leading to better health outcomes and potentially reducing the risk of death.
It’s important to know that the effect of MSC therapy on mortality is not direct and can be influenced by many factors.
Critical Limb Ischemia, MSC therapy, and mindful living
Individuals living with critical limb ischemia can experience debilitating pain and suffering, which can severely impact their quality of life.
Mesenchymal stem cells can help alleviate pain and discomfort associated with tissue ischemia by improving blood flow and suppressing inflammatory pathways.
Furthermore, MSCs can promote tissue repair and wound healing, improving the appearance of affected limbs and reducing visible signs of the condition.
As a result, it can contribute to a more positive self-perception.
Seeing tangible improvements in pain management, mobility, and overall well-being can alleviate anxieties associated with chronic pain, disability, and potential limb loss.
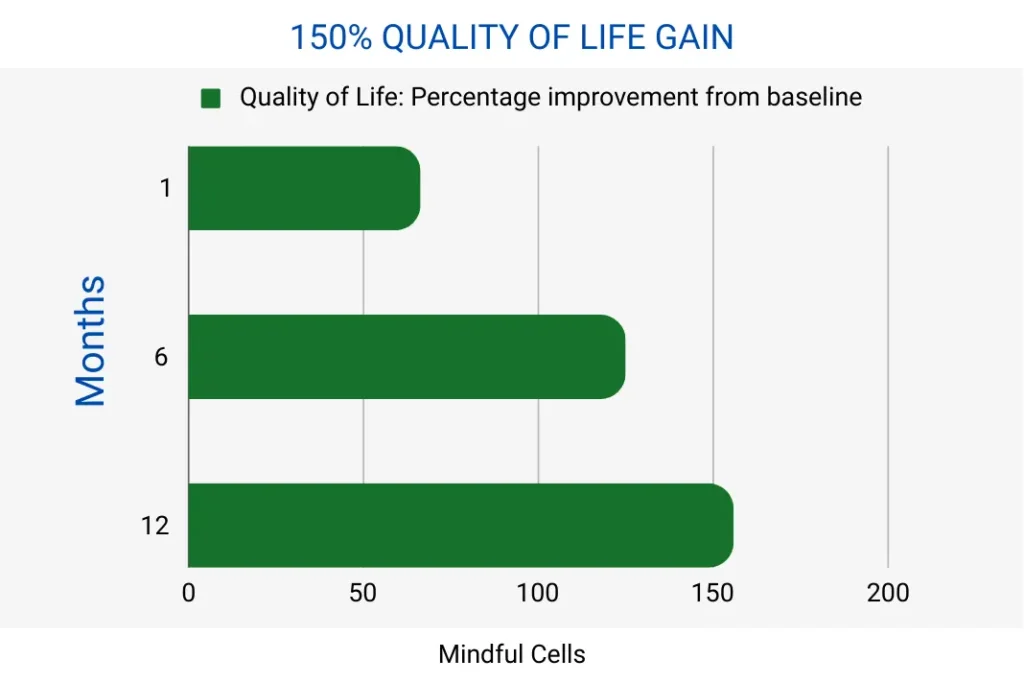
Yes, MSC therapy can improve the quality of life by 150% in 12 months.
Results demonstrated in a Phase III clinical trial with ‘No Option’ for treating critical limb ischemia patients.
Ultimately, MSC therapy increases energy levels and improves overall well-being.
FAQ
Peripheral artery disease is a problem in which the blood vessels that supply blood to your legs become narrow. It reduces blood flow to the legs, oxygen, and nutrition.
Critical limb ischemia is a severe stage of PAD. It occurs when there is significant blockage in blood flow to the legs.
CLI treatment involves injecting mesenchymal stem cells around the ulcer and calf muscle through an artery or muscle.
MSC-based therapy has been proven safe and does not lead to toxicity or abnormal differentiation in human clinical studies.
Moreover, the completed phase III study of CLI using MSCs has not induced any adverse effects or changes in the immunological profile.
MSC treatment can improve pain, blood flow, walking distance, and overall health over 12 months.
However, the success rate of complete cure or long-term outcomes is still being determined.
In addition, it is essential to note that the success rate of this therapy may vary based on patient characteristics and other factors.
More clinical research is needed to determine the success rate of MSC therapy for this condition.
The price of mesenchymal stem cell therapy for various medical conditions, including critical limb ischemia, depends on location, clinic, and specific treatment protocol.
According to data collected by The Niche, the general cost of stem cell therapy can range from $10,000 to $20,000, depending on the treatment and the provider.
To get accurate information about the cost of mesenchymal stem cell therapy for critical limb ischemia, you should consult your healthcare provider.
Finally, we recommend checking the approved clinical trials and products that meet your country’s regulations, such as the FDA.